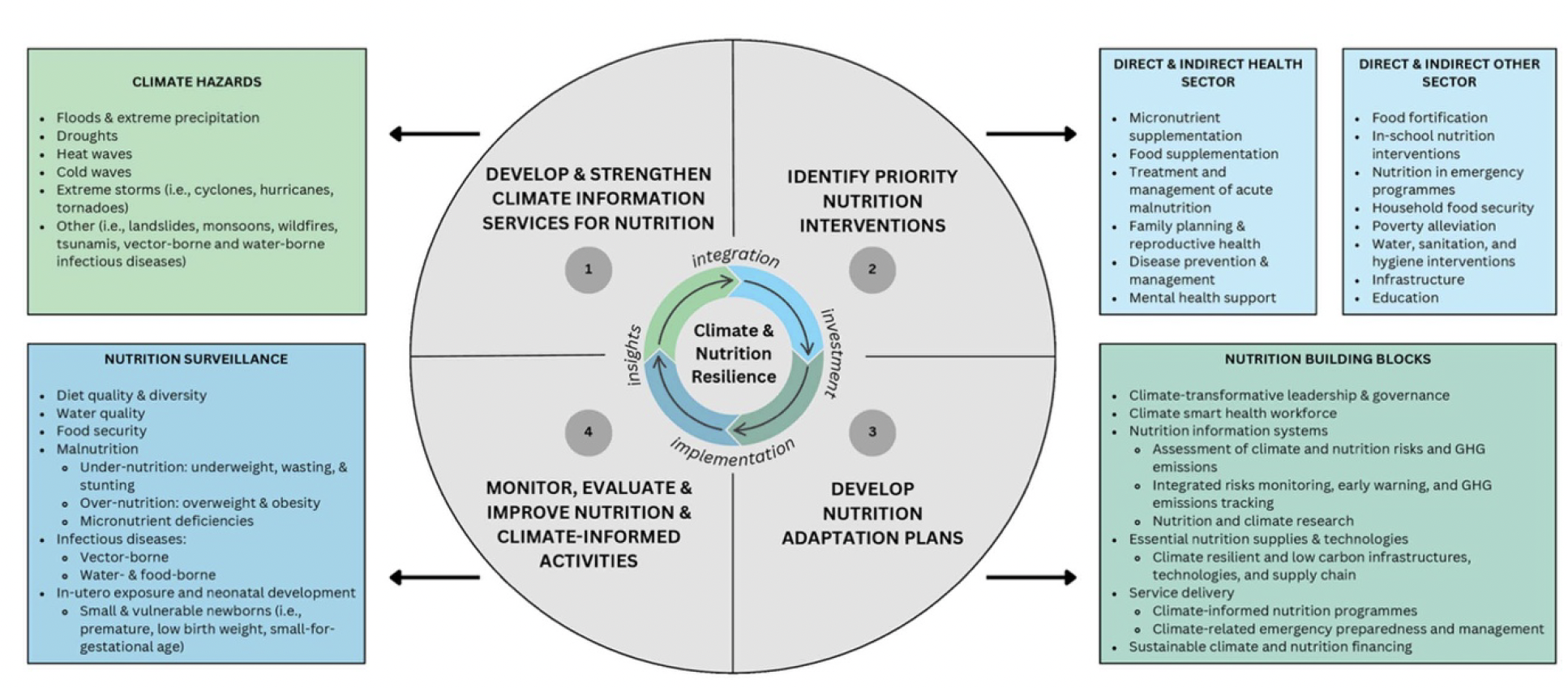
Recently, my team published a review exploring the intricate relationship among climate change, food security, and nutrition. Our study is rooted in the understanding that climate change significantly affects nutritional outcomes, particularly among vulnerable populations. We conducted a scoping review to identify and synthesize country-level programs that effectively integrate climate services into health systems and nutrition interventions. By doing so, we aimed to highlight the diverse strategies employed across settings, focusing on both direct and indirect interventions related to health and nutrition, while emphasizing the need for aligned actions across sectors.
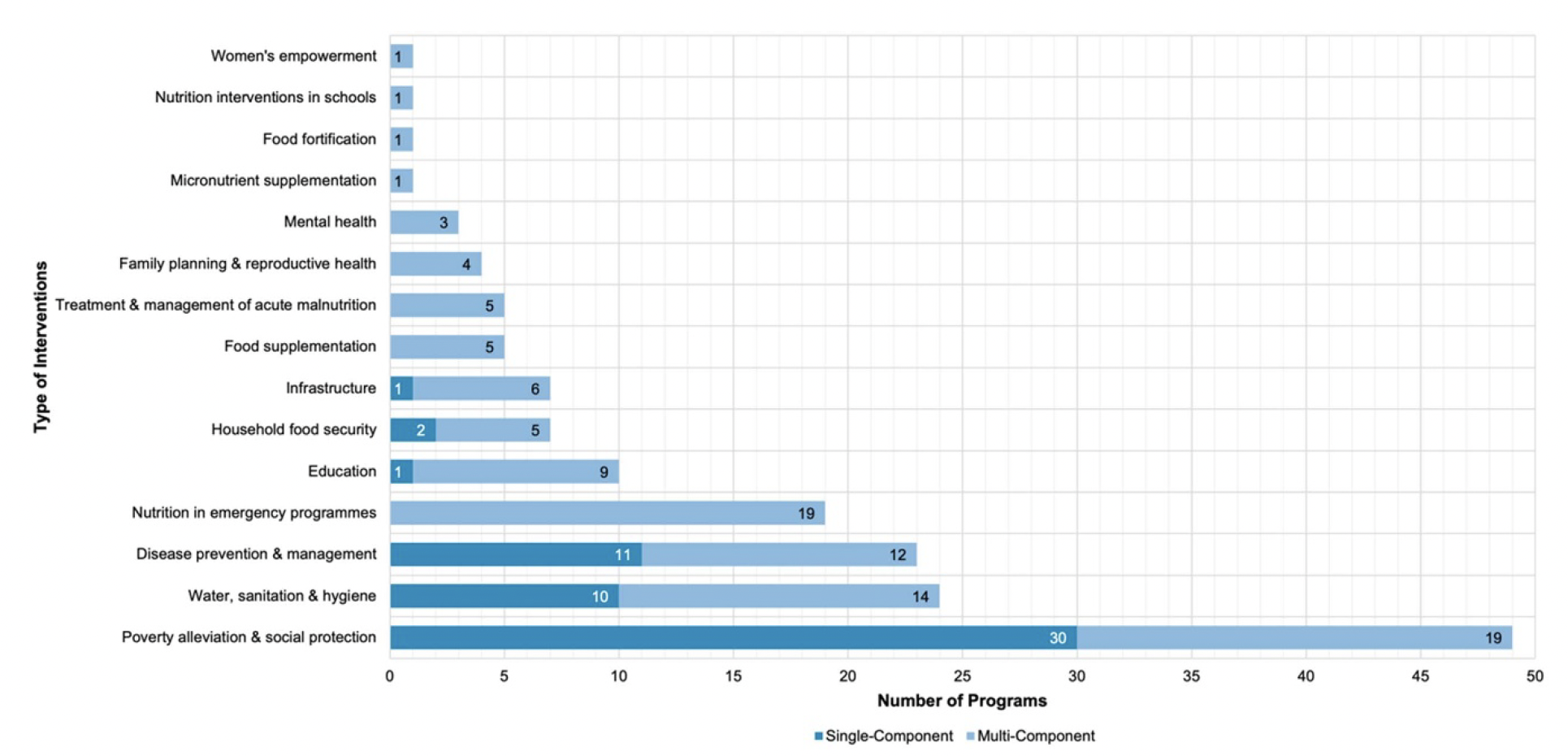
Our findings revealed 67 country-level programs that demonstrate innovative approaches to addressing the challenges posed by climate extremes, such as floods and droughts. We categorized these interventions using a framework that considers direct health-care strategies and various other sectoral strategies that affect nutrition.
Climate information and national nutrition planning and response conceptual framework (Carducci et al 2025)
Of these 67 programs, 42 were single-component, while 25 were multi-component, showcasing a variety of approaches to address the interconnectedness of climate change, nutrition, and health. For example, several initiatives specifically targeting women and children were noted, although many programs were more generalized, addressing broader populations affected by climate-related hazards.
Number of programs, by intervention type and component (Carducci et al 2025)
Among the specific programs mentioned, strategies varied widely across regions. In Bangladesh, for instance, multi-hazard climate information services were implemented to prepare for floods and droughts, while in Uganda, the Global Flood Awareness System was used to prevent disease, particularly diarrhea and malaria. Notably, Burundi's programs focused on anticipatory actions for flood management, incorporating both national and regional climate prediction efforts. Meanwhile, Zambia's initiatives used climate information to enhance malaria control efforts, underscoring the importance of integrating local and international resources to address public health challenges.
Interestingly, many initiatives were found to be more indirect, operating outside of traditional health interventions. This underscores the critical need for collaboration across sectors to prepare for and respond to climate-related challenges while improving nutritional outcomes for affected communities.
In conclusion, we advocate for strong partnerships between climate information service providers and stakeholders in the health and nutrition sectors. Our synthesis emphasizes that integrating climate services into nutrition policy and programming is not only beneficial but also necessary for developing resilient strategies to protect public health from the impacts of climate change. Through effective cooperation, knowledge sharing, and a focus on data-driven approaches, we can enhance our preparedness and response to the intertwined challenges of climate change and nutrition.